
Power and the Mind: Lacking power impairs thinking Writing in Psychological Science, Smith et al (2008) report that when randomly assigned participants are made to feel powerless they become worse at keeping on top of changing information, filtering out irrelevant stuff and planning ahead to get the task done.
I very much appreciated a recent post by Susan Giurleo on The Real Challenge of Health Care Social Media where she talks about the subtle shifts in power in a relationship that comes with health care professionals using social media. Social media requires more of an accessible, collaborative stance and certainly flies a bit in the face of the “mysterious therapy office.”
Social media will challenge therapists to carefully think through and articulate our boundaries for this new medium. That’s not a bad thing. However, as a trauma therapist and a trauma-informed therapist (they are not the same thing!), I am especially intrigued by any medium which helps at all to equalize some of the power differences that occur in therapy.
Trauma-informed practice requires that we examine all aspects of how we organize our services in light of what we know about how trauma affects people. Here’s a definition from The National Center for Trauma-Informed Care:
What is Trauma-Informed Care?
Most individuals seeking public behavioral health services and many other public services, such as homeless and domestic violence services, have histories of physical and sexual abuse and other types of trauma-inducing experiences. These experiences often lead to mental health and co-occurring disorders such as chronic health conditions, substance abuse, eating disorders, and HIV/AIDS, as well as contact with the criminal justice system
When a human service program takes the step to become trauma-informed, every part of its organization, management, and service delivery system is assessed and potentially modified to include a basic understanding of how trauma affects the life of an individual seeking services. Trauma-informed organizations, programs, and services are based on an understanding of the vulnerabilities or triggers of trauma survivors that traditional service delivery approaches may exacerbate, so that these services and programs can be more supportive and avoid re-traumatization.
Trauma, Power & Trauma-Informed Therapy
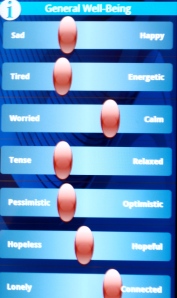
Understanding power is key to trauma-informed therapy. Most clients who are survivors of childhood trauma were abused by someone with power, someone who should have been trustworthy and then abused that trust. Therapists are authority figures who you are supposed to be able to trust, a characteristic we share with our clients’ abusers. Abuse involves the misuse of power–people who have been victimized feel helpless, vulnerable, and powerless. Healing from abuse involves recovering (or achieving for the first time) a sense of our power in the world. For this reason, a trauma-informed approach is based on the assumption that recovery from trauma must include collaboration and empowering clients whenever possible.
So What Does This Have to Do with Social Media?
Extending therapists’ reach into social media requires a level of transparency and accessibility that is a change from the traditional therapeutic model of the therapy room being a space set apart from the world. As Giurleo points out, this is a subtle shift in power dynamics. I hadn’t considered how much a difference this might make until I reflected on a recent conversation with a former client–I’ll call her Ann*. She remarked on the difference in my accessibility compared to more traditional/non-social media using therapists and noted that their limited accessibility made her interactions with them feel slightly “triggering,” that is, evoked some of her trauma-related symptoms. It’s not surprising that experiencing an authority figure/caregiver as inaccessible might evoke feelings of fear or abandonment related to experiences with caregivers from childhood. Her observation eloquently captures the impact of non-trauma informed practice and how a therapist’s willingness to use social media to enhance collaboration might shift some of those power dynamics. While some therapists might observe that such reactions are transference and provide important grist for therapy, I would point out that I rarely find that there’s a shortage of grist for therapy with people who grew up in abusive environments, and that people need to feel some measure of safety before they will take the risk of a connection with an authority figure after a lifetime of many authority figures who have either failed them or hurt them.
For all of the reasons discussed above, I think that with the proliferation of Web 2.0 in our society the trauma-informed therapist now has to consider moving into the world of social media. If your clients are there, you really need to be there too. If they aren’t there, they probably will be soon.
So How Should a Therapist Use Social Media?
Clearly there need to be boundaries on how this is done to protect confidentiality and to ensure that therapists get enough disconnected time so they can maintain wellness. In my own practice I have not used anything especially innovative, I have used social media/technology in only a few ways: allowing clients to text me information regarding appointment changes or to send me information we might need for an insurance form that they needed to verify at home; on request, reading a client’s blog entry; posting information that I thought might be helpful to clients on my therapy practice blog. I worked out any boundary issues with clients that needed to be addressed in the process of using those tools (“if you’re suicidal call me, do not text or email me anything that is a crisis”). Using these tools in limited ways hardly makes me an expert on all the most effective ways to do this. Fortunately, there are skilled, experienced people to help guide therapists in this process (e.g., see Mike Langlois, LCSW: How to Have a 100% HIPAA Compliant Online Presence, see Susan Giurleo, PhD’s posts social media for therapists), and–here’s a bonus–they, too, can be found in the social media world.
*”Ann” has seen this post and has given me permission to refer to her comments-and she may well decide to read this blog post.
Photo provided courtesy of Will Lion




You must be logged in to post a comment.